THE CLINICAL UPDATE | SUMMER 2020
Editor’s note – As we are “going to press” wildfires are raging in California caused by over 10,000 lightning strikes. We hope you and your loved ones are safe; we hope your homes are safe; we worry about the intersection of Covid-19 and the need for evacuations; we are incredibly grateful for firefighters and first responders. Our list serve (CSCSW@googlegroups.com) can be a place to share the impact on us and our clients, share resources and ways we can help.
Upcoming events
-
Saturday, March 07, 2026 10:00 AMKingscote Gardens Conference Room 140 419 Lagunita Dr. Stanford, CA 94305
-
Saturday, March 14, 2026 8:00 AMNew Village Girls Academy | 147 Occidental Blvd, Los Angeles, CA 90026
-
Tuesday, March 17, 2026 5:00 PMONLINE ZOOM
-
Saturday, March 21, 2026 9:00 AMONLINE ZOOM Meeting
-
Saturday, March 21, 2026 10:30 AMOnline ZOOM
-
Tuesday, March 24, 2026 8:30 AMOnline ZOOM
-
Wednesday, April 15, 2026 7:00 PMOnline ZOOM

Letter from our President, Monica Blauner, LCSW
These are very turbulent times: the Covid-19 pandemic, institutionalized racism, economic inequality and insecurity. The Diversity, Equity and Transformation (DET) Committee, chaired by Jaya Roy is leading the effort within our Society to advocate for and foster the professional development of clinical social workers from underrepresented communities, and to transform the Society’s culture to consciously embrace a commitment to promoting diversity and equity in clinical social work practice. As President of the Society, I am committed to this integral work and its goals. The DET committee has started a Clinical Consultation/Support Group for members who identify as BIPOC (Black, Indigenous, Mixed Race and Persons of Color); and to learn more please refer to the Real Talk column in this newsletter.
DISCOUNT
The Board, aware that many of our members may be economically impacted by the pandemic, decided to offer a coupon to all new and renewing members, for $20 off the cost of an upcoming CSCSW event. This will be good through this membership year, which ends June 30, 2021.
EVENTS
Since moving online there has been some confusion about why there are various charges for CSCSW events. To clarify, CSCSW has traditionally offered two types of CEU events (which are now being held online):
- District Meetings –are free to Members. Speakers receive no fee. Nonmembers pay a fee based on CEU’s. We are committed to continuing to offer free CEU’s for these presentations as an important benefit of membership.
- Workshops –members pay a reduced rate (e.g. Law and Ethics, Suicide Prevention). Speakers are paid. The cost of these events is based in part on the speaker’s fee. Workshops are an important source of income for the Society.
Upcoming Workshops: For details and to register, go to our website: www.clinicalsocialworksociety.org
- Suicide Prevention: Saturdays, October 3rd and 10th, 9:00 am to noon
- Law and Ethics: Saturdays, November 14th and 21st, 9:00 am to noon
- The Art of Group Facilitation Using ZOOM - (TWO SESSIONS - REGISTER FOR ONE): September 26 & October 24
Upcoming District Meetings: For details and to register, go to our website: www.clinicalsocialworksociety.org
- The Art of Psychotherapy: What do you do after you say hello? Beginnings & Beyond: Sunday, August 30th at 10 am – Online ZOOM Webinar
- Getting Unstuck: The Promise of Psychedelic Therapies: Wednesday, September 16th from 7:00 – 8:30.
- Anesthetics, Magnets and Electricity in Psychiatry: Wednesday, November 4th from 6:30 – 8:30.
Ongoing groups (free for members):
- Real Talk – biweekly: Real Talk is a clinical consultation/support group developed with the oversight of the CSCSW's Diversity, Equity and Transformation (DET) Committee, the purpose of which is to provide a space for clinical social workers who identify as being Black, Indigenous, Mixed Race, or Person of Color (BIPOC) to meet on a monthly basis. The focus of this group is to provide an opportunity for networking, building solidarity, exploring intersectionality and decolonizing our practice. Please note that this group does NOT provide supervision to its members and no CEU’s are offered.
- Telehealth – monthly: Open consultation/support group for CSCSW members to discuss topics, questions, concerns, creative solutions, etc. regarding the use of Telehealth, particularly in response to the COVID-19 pandemic. Previous meetings have included discussions around the use of different telehealth platforms, how clinicians are approaching their work with children, teens and TAY through telehealth, navigating insurance, resource sharing, etc.
MEMBERSHIP
Our membership is steadily increasing. We had 600 members at the beginning of June (the most we’ve had in the last five years) and renewals are coming in at a very fast rate. This is a testament to the value of the Society to its members, particularly during the pandemic when a large portion of the profession moved online.
Please update your Member Profile, if you haven’t already done so. Last year we began collecting demographic information on our members. Since this information is included in the Therapist Directory, it can help in finding appropriate referrals for people with specific needs. Also, please consider volunteering to be a Mentor for someone new to the profession. Mentorship is an extremely rewarding aspect of professional development. Please check the appropriate box in your member profile and write a short statement about yourself to help potential mentees find a suitable match.
Jannette Alexander Foundation
We are pleased to announce this year’s winners of the Jannette Alexander Foundation scholarship for clinical excellence (see our recipients here). We are very grateful to Karen Druker for her generous contribution to the scholarship fund in honor of our past President, Leah Reider. Please remember that donations to JAF are tax deductible, and will allow us to continue to support graduating clinical social work students.
GET INVOLVED!
CSCSW is a volunteer run organization that provides opportunities for leadership and resume building experience. Be an active member of our professional community - give a presentation, organize a peer consultation or study group, join a committee, suggest a speaker! Being online also presents the opportunity to expand your professional community around the state. The Society will provide technical support. If you have any ideas or questions you’d like to discuss, feel free to contact me at Monica@Monicablauner.com
Membership renewal for fiscal year
| TO UPDATE YOUR ONLINE PROFILE
Limited information is automatically shown on the Therapist Finder. You can change your privacy settings to have your information shown to the public or to CSCSW members only. TO CHANGE YOUR PRIVACY SETTINGS
|
JANNETTE ALEXANDER FOUNDATION
Jannette Alexander Scholarship Recipients
Kean Flowers
 Kean has ben working within social work for three years and has interest in working with children, adolescents, transition-age youths. He currently interns at The Guidance Center, Long Beach where he provides individual psychotherapy, group psychotherapy, and facilitates presentations on socio-emotional learning to students and school staff. Kean is devoted to working with minority populations in schools to reduce the disparities seen in these children’s mental health and educational outcomes. He is a strong advocate for transforming school climate through destigmatizing mental health and increasing culturally-sensitive, accessible mental health practices in schools; both of which are critical factors in closing the mental health and educational gaps in marginalized communities. As a former collegiate athlete, Kean enjoys drawing from his love for basketball and kinesiology to provide creative mental health interventions to clients. Eventually, Kean aspires to attain a leadership role within schools to foster a school climate that advances preventive efforts for mental health disorders and school-wide mental health services.
Kean has ben working within social work for three years and has interest in working with children, adolescents, transition-age youths. He currently interns at The Guidance Center, Long Beach where he provides individual psychotherapy, group psychotherapy, and facilitates presentations on socio-emotional learning to students and school staff. Kean is devoted to working with minority populations in schools to reduce the disparities seen in these children’s mental health and educational outcomes. He is a strong advocate for transforming school climate through destigmatizing mental health and increasing culturally-sensitive, accessible mental health practices in schools; both of which are critical factors in closing the mental health and educational gaps in marginalized communities. As a former collegiate athlete, Kean enjoys drawing from his love for basketball and kinesiology to provide creative mental health interventions to clients. Eventually, Kean aspires to attain a leadership role within schools to foster a school climate that advances preventive efforts for mental health disorders and school-wide mental health services.
Rebekkah Gong
 Rebekah Gong is an MSW candidate at the University of California, Berkeley’s School of Social Welfare. Prior to Berkeley, she has worked in mental health service and gender equality advocacy for vulnerable populations for years, including domestic violence survivors and sexual minorities. She holds a psychological counselor license in China, and a postgraduate diploma in gender, sexuality, and relationship diversity therapy from the UK. She provides clinical services in English and Mandarin.
Rebekah Gong is an MSW candidate at the University of California, Berkeley’s School of Social Welfare. Prior to Berkeley, she has worked in mental health service and gender equality advocacy for vulnerable populations for years, including domestic violence survivors and sexual minorities. She holds a psychological counselor license in China, and a postgraduate diploma in gender, sexuality, and relationship diversity therapy from the UK. She provides clinical services in English and Mandarin.
Nigel Pacheco

Social work became a personal interest of mine not through professional or academic interest, but through intervention. At 19 years old I was in a challenging and life-endangering position. I was expelled from a university following my freshman year performance, I was in the throws of addiction, and I was completely unemployable. It was at this time that I was blessed to have my first interaction with clinical social workers. Through the experiences that I had seeking my own mental wellbeing, the fire for human service was lit within me.
Academically, I had to start again at the community college level. I then moved to USC where I graduated on the Dean's List with departmental honors for my research in sociology. Throughout my academic career I volunteered as a mentor at Oakwood Family Treatment Centers, providing support and guidance to adolescents who were experiencing behavioral and substance abuse issues.
Following my graduation, I eventually started working as a residential counselor at Five Acres. My work there taught me volumes about crisis, behaviorism, and patience as a professional helper. While working at Five Acres I applied to the USC School of Social Work because I knew my heart was set on clinical practice. I was lucky to be accepted and awarded the Dean's Leadership Scholarship which allowed me to pursue my education and truly begin my career as a social worker.
My first year field placement as a social work intern was with a small organization in South Los Angeles called the Francisco Homes. Here I provided clinical case management and brief therapeutic interventions to men who were on parole following life sentences in prison. I was honored to be able to share space with clients who had such unique forensic experiences and feel grateful and enriched to be exposed to their singular perspectives and positionality.
My second year, and current, field placement is at USC University Health Center in the Counseling and Mental Health department. Here I provide brief therapy to undergraduate and graduate students who present with issues ranging from anxiety and depression, to academic difficulties, to long standing family issues and trauma. I am being provided with truly top-shelf training and supervision that is growing me clinically and as a person. I am able to explore the psychodynamic avenues where I feel clinically at home as well as providing skills and strategies that my clients are able to use and benefit from immediately.
JAF Donation in Honor of Leah Reider
By Monica Blauner, LCSW
 CSCSW thanks Karen Druker for her extraordinarily generous contribution of $6,000 to the Jannette Alexander Foundation (JAF), which she gave in honor of Leah Reider, past President of CSCSW. The fund provides scholarships to graduating social work students based on clinical excellence.
CSCSW thanks Karen Druker for her extraordinarily generous contribution of $6,000 to the Jannette Alexander Foundation (JAF), which she gave in honor of Leah Reider, past President of CSCSW. The fund provides scholarships to graduating social work students based on clinical excellence.
Karen Druker is the widow of Leah’s late brother, Dr. David Druker, who was the CEO of the Palo Alto Medical Foundation. She is a talented artist whose work has won national, state, and local awards and has been exhibited in many galleries. Karen was president of the Los Altos Art Docents and recently retired from being exhibits chairperson for the Santa Clara Valley Watercolor Society. She founded and was chair of the Los Altos Hills Art in Public Places Committee. In addition, Karen served as Curator of Art for the Baylands Ecocenter and the Town of Los Altos Hills. Karen is very philanthropic and donated a shelter and playground to her Iowa hometown.
Leah Reider, LCSW, is a past President of the Society and the winner of the Society Member of the Year Award for her outstanding contribution to CSCSW. Leah served twelve years on the CSCSW Board and two terms as President during the organization’s most challenging time. She single handedly shepherded the organization from near dissolution back to health. When faced with possible need to close the organization, she spent countless hours in discussions about state of the society and organized a weekend retreat devoted to planning its future. She brought in long time members as well as a new generation of leaders, who after considering a number of different options, decided to revive the organization. She subsequently solicited new board members, planned and hosted meetings, supported the District Coordinators in planning local District Meetings, revived the Jannette Alexander Foundation Scholarship, reinstituted the Mentorship Program and increased overall membership. Under her stewardship new member benefits were instituted, including the Listserv, the BBS Liaison and Supervisor List to attract a new generation of clinical social workers to the organization and ensure its continuity. Leah went above and beyond in terms of the many hours she has devoted to reviving the Board and the Society, all the while managing a full-time clinical practice serving children and adults.
Leah received her BA in psychology from Wellesley College in 1969 and her MSW from UC Berkeley in 1971. She has worked in the public and private sectors, providing consultation to Castilleja School, Family Service Association of the Mid-Peninsula, and The Children’s Health Council; and provided psychotherapy for Jewish Family and Children’s Services and Contra Costa County Social Service Department. Her clients have ranged in age from children to seniors.
Screen Play: Play Therapy Moves On-line
 By Jeannette Harroun, LMFT, RPT-S
By Jeannette Harroun, LMFT, RPT-S
COVID-19 shifted many of us from our familiar offices and playrooms to on-line sessions. The transition happened quickly, leaving many therapists scrambling to provide therapy services while simultaneously learning to manage an array of challenges. These ranged from learning and at times, troubleshooting teleconferencing platforms and other communication technology, along with dealing with new confidentiality issues. We also had to devise new ways to interact with and engage clients, while managing our own change-challenged feelings.
Session Structure/Setting up the Environment
Therapy is always about creating a safe and comfortable environment in which clients can freely express themselves. In play therapy this includes confidentiality, the structure provided by both our presence and our physical office space, and the therapeutic relationship. Together these serve to create a safe container that allows children and teens to play in creative ways and explore and process thoughts, feelings and behaviors that are not always comfortable. Finding ways to create the container in lieu of physical office space is the first step in a successful teleplay session.
Directive play works well in a teleplay format and, even if therapists want to be more non-directive, can be useful to establish session structure and help clients understand what will happen. Parents can also help create structure and space for therapy by assisting in setting up and troubleshooting technology and ensuring that the space is confidential.
When working with younger children, using a modified approach to child centered play based on recommendations by Dee Ray, Ph.D. and Rise Van Fleet, Ph.D. also works well both for creating structure and providing services. This includes training parents in the empathy and limit-setting skills used in filial therapy to support in-session interactions and help with child self-regulation. Parent support and coaching is also provided after each session. Filial therapy is the combination of child-centered play and family therapy developed by Bernard and Louise Guerney in the 1960s. Other child-centered elements that can be utilized in telehealth play include offering activity choices and encouraging children to lead activities where possible. For example, one of my young clients loves to end the on-line session by leading a game of “Puppet Says” (Simon Says). She uses stuffed animals in lieu of puppets as she provides instructions that her mother and I must follow.
Finally, creating a rough “lesson plan” for each client that includes activities for check-in, engagement, and a transitional activity to end the session (important for younger children) is another way to create session structure. Having a plan allows me to consciously connect therapy goals and learning with activities, and gives me multiple activities to choose from so I can switch gears easily as needed on a given day.
Intentional Presence Supports Emotional Connection
Many therapists acknowledge finding it more difficult to feel emotionally connected across screens. It simply is more difficult and takes more effort on our part. Normally we rely on our observation of both verbal and non-verbal cues; however, during telehealth we have little to no non-verbal information available to us. This does not mean it’s impossible to feel connected, it just means that the lack of sensory information requires a more intentional presence as the means to create and experience a “felt sense” in a teleplay session. It takes more effort, something that in addition to being on-line for long periods of time tends to be exhausting. Zoom fatigue and therapist fatigue are real and self-care is even more important right now.
The Challenge of Keeping Clients Engaged
Keeping clients engaged on-line is often more challenging, as is finding ways to creatively support their ability to explore and process thoughts, feelings and behaviors, especially when using less familiar tools such as read-aloud books (Youtube) and on-line games and activities. Even familiar activities like drawing, puppets and playdoh don’t always maintain engagement as children get bored or are tired after a long day of Zoom school and homework.
Technology issues (bandwidth, loss of Internet connection, device issues) and lack of or challenges to confidentiality can also serve to disrupt client engagement. When clients aren’t engaged, they are more likely to become distracted and bored.
Building your own toolkit of go to activities as well as being alert to client moods and needs can make a huge difference in helping clients not only maintain interest in the session but also be more willing to work therapeutically. I keep in mind that many times clients have already been on-line for hours, whether it’s doing schoolwork or playing and talking with friends. They may be tired, making it difficult for them to sustain interest. When clients - especially younger ones - become fidgety and restless, I change activities to something active such as scavenger hunts, yoga or a “freeze dance.”
Involving Parents in Telemental Health
Including parents in play therapy, particularly when connecting over screens, can be very helpful. Most children enjoy having their parents’ undivided and playful attention and parents also can learn about their child in new ways. Many report that the experience has deepened their relationship with their child. However, as beneficial as involving parents may be, it is important to assess how the parent’s presence impacts the child in the home environment. Some parents struggle to learn and use therapeutic play skills. There are many reasons for this, but when a parent isn’t able or willing to shift, their participation in therapy may be detrimental. When parents interject their own rules rather than honoring the child-centered rules of “special play time,” increased anxiety and confusion may ensue for the child who is desperately trying to reconcile two different sets of rules about therapeutic play.
Intervention Toolbox
It always helps to have a toolbox and many of the directive activities such as puppet play, bibliotherapy, and art already used in therapy easily translate to teleplay with a little preparation. Where video can be used and shared, Youtube has many resources – informational videos, books read aloud for kids and movement or mindfulness activities. Just as some kids move from activity to activity in the playroom, I like to have an array of options available to keep clients connected and engaged in the work of therapy. I also find it helpful to talk about boredom and distraction in a matter-of-fact manner so children are able to express their needs more comfortably; this reduces acting out behaviors.
The following is a list of some of my “go to” resources for teleplay.
Bibliotherapy: Books support cognitive development and are a resource for skill building and learning – all things that translate well to teleplay.While I do read to clients myself, it is helpful to use Youtube ‘read aloud’ videos since the video portion makes it easier to see pictures and follow the story. Many of the books we use in our offices are available as “read alouds.” I have found many favorites and developed new ones. Some new ones include books by Tom Percival (Ruby Has a Worry, Ravi’s Roar about Dealing with Anger and Big Feelings; and Perfectly Norman about Self-Acceptance) and Ashley Spires (The Thing that Lou Couldn’t Do and The Most Magnificent Thing – two takes on perspective, effort and growth.)
Art, Bubbles and Other Therapeutic Activities: These kinds of activities release physical energy, provide safe, metaphoric opportunities for emotional expression and a sense of control over the environment.
My clients and I often draw together on the Zoom whiteboard or on a drawing website like Sketch.io. Drawings might be Color Your Feelings, doing a Circle of Control or a squiggle drawing that we do together. For art activities done at home that require advance preparation, parents are asked to provide the materials, or I purchase and mail the child a package of supplies. Typically, these would be things like bubbles, cotton balls, crayons, and playdoh.
Theraplay Activities: These are great activities for increasing parent-child connection and attachment, and I use them frequently in teleplay when parents are available. There are many descriptions of Theraplay activities available on-line. Kids enjoy activities like bubble tennis, bubble breathing, thumb wrestling, pillow balancing or creating a pillow jumping maze, low and high fives, and M&M (or cotton ball) hockey. A number of these activities work well with older children too.
Scavenger hunts: No supplies needed! These can be done in a single room, in the client’s house or outside. They are great for kids who really need movement or sensory play. These are enjoyed by teens and middle-schoolers as well as younger children. I always ask the client (or parent) to either do the hunt in one room where I can see them or take me along on a smart phone. There are lots of ideas on Pinterest. Some that I use include:
- Teletherapy Scavenger hunt (The list is on Pinterest and usually shows up in as the first image when searching on the words “teletherapy scavenger hunt.”)
- Sensory Nature Scavenger Hunts (Many lists of these on Pinterest)
- Therapeutic Scavenger Hunts –This packet can be found by searching on the words “Play Therapy scavenger hunts: free download. “
Word art: https://www.wordart.com . This is a free website for creating beautiful word clouds from text. Clients can choose the words, colors, font styles and cloud or image shapes to reflect feelings, moods, and thoughts. I use this via a “share” screen in Zoom and find it very useful in helping clients go deeper, creating links between events/triggers, feelings and the embodiment of feelings. As an example of use, one young client told me that she felt “blah.” In exploring this using Wordart we talked about what she’d been doing during the week and adding feeling words to the events and situations she described. The activity phrases and feeling words were input as separate lines with their own corresponding colors. She chose a font, a shape and even the direction of the words. Blah suddenly went from “I don’t know” to bored, missing friends, lonely, frustrated with shelter in place, and no place to put my feelings. We were then able to explore these feelings more deeply.
Movement activities: These types of activities keep clients engaged while supporting body awareness. I’ve also found them useful in helping child and teen clients understand feelings embodiment by talking about where they feel the energy of their emotions. There are many more movement activities available on Youtube for kids and adults. Some combine movement and mindfulness. The Go Noodle website: https://www.gonoodle.com/ is an excellent resource for this. Youtube also has a good Freeze Dance video.
In addition, familiar games like Simon says and Red Light/Green Light are a great way to re-engage or re-direct elementary age kids, particularly when they are bored and losing interest in the therapy session. I suggest kids hop rather than run when in small spaces. Movement is sensory so it helps with calming and self-regulation, as well as helping to increase focus, get rid of excess energy, and improve impulse control.
Mindfulness activities: While mindfulness activities including guided relaxation and yoga can be done without a video as the therapist demonstrates and does the activity with the client, I’ve found many clients prefer having a video to follow. For these clients I find activities on either the Go Noodle website noted above or on the Go Zen Mindfulness channel on Youtube.
Games: Board and card games generally support cognitive development, strategy, problem-solving and social skills. They are also a resource for connection.
There are a wide array of games that can be played with clients on-line either through a shared screen or by creating a private room or link so that client confidentiality is maintained. Cardgames.io is a site with many familiar card and strategy games ranging from Crazy8s and Go Fish to Backgammon and Chess. It is free and the multiplayer set up is straightforward allowing you to create a ‘private table’ that only your client may enter. Skribbl.io is another client favorite. This is a Pictionary-style game where players take turns making drawings so that the other can guess the word. You can create your own custom word list and use it exclusively. It’s a great intervention for talking about communication and perceptions. A favorite example is the time a client chose the word “iron” to illustrate. After choosing the word, he wasn’t sure how to communicate it to me and began drawing a rectangle over and over. When the timer ended without a correct guess on my part, he said he’d been drawing a Minecraft iron ingot. Since I don’t play Minecraft I didn’t associate the image with the word – I associate it with a clothing iron, something the client had never seen. This led to a wonderful conversation about communication and assumption.
Gamification of real life. Kids also respond well to the concept of “gamifying” which is a learning management/productivity strategy that can be used at any age. Essentially the idea is to turn even the most mundane tasks into a game which in turn creates motivation and serves to increase the likelihood that the person will accomplish what they need to accomplish. There are numerous articles about this as well as apps such as Habitica and Epic Win that can be useful for motivation, productivity, and learning management.
In addition to more structured interventions I encourage clients to show me their world. I’ve seen their homes, rooms, yards, and pets. I’ve had them teach me to play their videogames and seen drawings and screenshots of their videogames and videogame characters and those of their friends.
Dealing With Telehealth/Teleplay Challenges
Challenging behaviors do occur – kids leave the room or say they don’t want to play – but more often than not they can be re-engaged through use of empathy and changing up the activity. In addition, when a client is struggling to engage, I always try to think about what might be motivating the underlying discomfort. Does the game or activity feel too difficult? Are they restless and needing to move? Is this a client who is only in therapy because parents are requiring it? In the first case I might change to an easier game or activity; in the second, I suggest a scavenger hunt, bubbles, playdoh or movement activity; and in the third, I look for ways that the client can express his or her feelings about having to be in therapy – drawing, scribbles, colors, Wordart etc.
Although I regularly think about therapy goals, objectives and expectations, I have found that teleplay necessitates re-examining and updating them to reflect changes to client environments and concerns. For example, anxiety and anxious behaviors triggered and sustained by heavy school workloads and overscheduling may have shifted or even gone away in the face of reduced assignments and removal of after school activities; however, feelings of loneliness, sadness or even depression may have increased. It may be necessary to shift the goals (and thus the therapy interventions) to meet new needs, or simply step back and focus on relationship while re-evaluating what is needed. This often alleviates the problem of client engagement and results in greater interest and progress.
In summary, teletherapy and teleplay can work well. There are challenges but also solutions. Teleplay uses our therapeutic skills including relationship building, compassion and empathy. It also requires us to adapt creatively to provide support and identify interventions that can be directed or done effectively through a screen to support our clients’ needs.
RESOURCES:
- Filial Play Therapy Training:
- Growth Through Play Training Associates: https://growththroughplaytherapy.com/training.html
- Rise Van Fleet: http://risevanfleet.com/shop/product-category/training/play-filial-therapy-workshops/
- Center for Play Therapy (University of North Texas)*: https://cpt.unt.edu/child-parent-relationship-therapy-certification *UNT refers to filial therapy as “Child-Parent Relationship Training”
References
Books:
- Stone, Jessica Ed. 2019. Integrating Technology Into Modern Therapies. A Clinician’s Guide to Develops and Interventions. Routledge, New York, NY
- Van Fleet, Rise. 2014. Filial Therapy-Strengthening parent-Child Relationships Through Play, 3rd Ed. Professional Resource Press. Sarasota, FL
Articles:
- Brandal, Benjamin. August 1, 2016. Productivity. Why You get More done when you gamify your life.: Retrieved on July 17, 2020 from https://blog.trello.com/get-more-done-gamify-your-life
- Denbrough, Heather F. LCSW, RPT-S. June 20, 2020, Dimensions of Successful Telehealth Play Therapy with Young Children. Retrieved, July 1, 2020 from https://synergeticplaytherapy.com/dimensions-of-successful-telehealth-play-therapy-with-young-children/
- Drinko, Clay Ph.D. September 18, 2019. How to be more Playful: Gamify Your Life. Retrieved on July 17, 2020 from https://www.playyourwaysane.com/gamify-your-life/
- Ray, Dee, Ph.D. March 2020. Child-Centered Play Therapy and Telehealth. Retrieved June 15, 2020 from https://www.artandplaytherapytraining.com.au/files/CCPT%20&%20Telehealth.pdf
Websites and Social Media:
- Levine, Peter, Ph.D. Felt Sense. August 16, 2019. Youtube interview. https://www.youtube.com/watch?v=ZBLe84U7AaM
- Facebook.com. Tele-PLAY Resources and Support Group.
Jeannette Harroun, LMFT, RPT-S has a private practice in Lafayette, CA. She specializes in working with children, teens, and families, helping them build stronger relationships and address concerns including anxiety, self-regulation, attachment, trauma and parenting. Her play therapy training includes child-centered play, sandtray and filial therapy as well as parent education. She supervises for the Wright Institute and offers play therapy training classes. She can be reached at jeannette@bayarea-counseling.com or at (925) 890-7478
A Letter to Parents: Supporting Elementary School-Aged Kids During COVID-19
By Leah Reider, LCSW
During the current outbreak of COVID-19, parents are overwhelmed. You are probably managing household responsibilities, trying to keep your kids from killing each other, working from home, and more. Now you are having to figure out what to do with your children during the summer, when many of the traditional activities are not open. Give yourself permission to let go of judgments that you aren’t doing it “right” or doing enough. Here are some ideas to help manage your children’s stress. Choose the ones that resonate most for you. Know that no one could implement all of them at once.
Honest Communication
Be honest, but don’t overshare. If your children express fear that you or they will get sick, tell them you are doing everything you can to stay well and to help them stay well. It is best not to promise them that no one you know will get sick. If someone does get sick, your kids won’t believe you the next time. You can say that it is very unlikely that any of you will get sick because of the measures you are taking.
The information you give should be developmentally appropriate. Be more concise and concrete with younger children. Don’t give too much information at once. If you don’t know the answer, it is OK to say so and that you will find out. You can go to the CDC website for information. In the absence of information, children often imagine situations far worse than reality. It is a good idea to avoid watching the news when your children are in earshot, as this may only make them worry more.
If they ask, tell them that COVID-19 is a new virus. Doctors and scientists are still learning about it. Some people have been pretty sick, but most people will be OK, especially kids. If you get sick, it does not mean that you have COVID-19. You may just have a cold. Scientists are working on medicine that will help people get better and on a vaccine that will keep people from getting COVID-19. We can do things to help protect us.
Let children know what they can do to help prevent getting COVID-19. Review and model basic hygiene, such as handwashing multiple times a day for at least 20 seconds, covering your mouth with a tissue or your elbow when sneezing or coughing, and waving at friends through a window or blowing grandma a kiss.
Try to remain calm and reassuring. Kids pick up on your feelings. If you are feeling anxious, try not to talk about your concerns within earshot of children. Step away and take a break if you can. If they do sense that you are worried, talk to them about how that makes them feel and let them know that you can understand that seeing you worry may make them worry. Let them know that it is normal to worry sometimes and that they can always come to you with their worries. It might be helpful for you to tell them something that you do to calm yourself when you are worried. This could be taking deep breaths or talking to another adult about your worries. Then you can help them to come up with strategies which could help them with their worries.
Coping
Try to keep regular routines as much as possible. Keep normal meal times, bedtimes, and chores. Kids, especially younger ones or those who are anxious, benefit from knowing what’s going to happen and when. Most people are feeling a loss of control right now. Being able to have regular, predictable routines make children (and adults) feel better. Daily routines should include supportive relationships, exercise, healthy sleep, and nutrition.
Do some distracting. Ideas for activities to do with your children include playing games, doing art projects, watching movies, baking favorite desserts, taking a family walk or bike ride, doing yoga, dancing, playing music, etc. Of course, you are probably much too busy to do all of those activities. Just remember that it is important to have some fun with your kids. Be silly and laugh. Remember that play is part of a kid’s “job.” Opportunities for creativity and play are critical for a child’s development. It’s also important for everyone’s mental and physical health to go outside and get some exercise.
Help children talk about their feelings. You could ask what they were feeling when they found out about COVID-19 and what they are feeling now. You could even write down a list of their feelings or draw pictures of people with particular feelings. With younger children, you could take out a figurine and ask what this boy or girl was feeling when they heard about the illness. You could say things like, “I bet that boy was scared” if you think that is what your child is trying to tell you.
Another idea to help children talk about their feelings is playing a game called “Rose, thorn, bud” at dinner. Each child talks about their rose of the day, which is a nice thing that happened to them; their thorn of the day, which is something difficult that they had to deal with; and their bud, which is something they hope will happen or an idea to be explored. This can lead to a wonderful family discussion and will help everyone to feel included.
Whenever possible, network via Zoom, FaceTime, etc. with friends and relatives, or write letters to Grandma and Grandpa. Perhaps a grandparent could read a story to a child on Zoom. Having drive-by or social distancing visits with friends and relatives can feel much better than doing Zoom or phone visits. Socializing plays an important role in regulating mood (both yours and your child’s). Of course, it is important to pay attention to the guidelines put in place by the health authorities in your area.
It makes people (adults and children) feel better when they can do something for someone else. Perhaps your children could make a card for a medical professional who is on the front lines dealing with people who are ill with COVID-19.
You are probably anticipating the new arrangements which you and your children will have to deal with around returning to school in the fall. Some school districts are planning to have students return part time and others plan to continue with distance learning exclusively. You are already aware of the challenges of helping young children to navigate the complexities of distance learning and may not be looking forward to facing this situation again. If you have a partner, hopefully you can share these responsibilities. Do not hesitate to contact your child’s teacher for help. Unless you were trained as a teacher, you are not expected to have the expertise to know how best to help your child.
Watch for changes in behavior. These changes may include physical complaints, tantrums, defiance, separation issues, difficulty going to sleep, wanting to sleep with parents, eating less than normal, and other symptoms which indicate a change from usual behavior. These changes are usually symptoms of anxiety. Find a time when you can talk to your children about their worries. If your child has seen a therapist, contact the therapist to see if you can set up some video sessions.
Self Care
Be kind to yourself. Don’t expect yourself to be a perfect parent. It’s OK if your kids watch TV more than usual. Managing your own stress response will help you and your children. Take care of yourself as much as you can. Go for a walk, do yoga, cook, exercise, take a nap, or meditate. If you have another adult at home, agree that you’ll trade off when it comes to childcare. This will give you time for self-care. If you have a therapist, continue to talk with that person. Consider starting therapy if you are having difficulty managing your stress level.
OTHER RESOURCES
- Manuela Molina Cruz has written a short online book explaining COVID-19 to young children and helping them to express their feelings.
- Access the “California Surgeon General’s Playbook: Stress Relief for Caregivers and Kids During Covid-19” here. The last section, entitled “Self-care Template for Kids” has a list of goals your family can set together to support your children’s health.
Leah Reider, LCSW has been treating children, adolescents and adults in her practice in Palo Alto since 1986. She was on the board of CSCSW for 12 years and served as president for 4 years. She can be reached at Leah.Reiderlcsw@gmail.com and 650 996-7602.
Utilizing Somatic Therapies to Manage Collective and Individual Trauma

by Emily Plain, MSW
We’ll get through this, but we need each other – Peter Levine, PhD, creator of Somatic Experiencing.
2020 may be described as a time of collective trauma: a time when “cataclysmic events have shattered the basic fabric of society” resulting in a “horrific loss of life…and a “crisis of meaning” (Hirschberger, 2018). Further aggravating the situation is the need to physically distance at the very time we need to connect for support and band together in order to stop the spread of a virus and prevent our health care system from becoming over-burdened. The COVID-19 pandemic and social injustice have caused civil unrest and disruption in our daily lives, and, for some, the unremitting stress may lead to an experience of trauma. As such, it is more important than ever to utilize trauma informed therapies to foster the resiliency needed to navigate our way through this time of uncertainty, change and crisis.
As clinicians we can provide clients with interventions and coping strategies during times of intense disturbance to mitigate a stress reaction and prevent a traumatic response. We promote individual and collective empowerment by creating a safe container where clients feel secure enough to attach, integrate and heal. Still, how can we effectively assist a client whose body has become an unsafe container? Dr. Peter Levine, founder of the therapeutic intervention known as Somatic Experiencing explains that “trauma is not caused by the event itself but rather develops by the failure of the body, mind, sprit and nervous system to process extreme adverse events” (Neukrug, 2015). Therefore, it may be very helpful to utilize somatic interventions that incorporate top down and bottom up processing to completely discharge trauma so the body can re-balance and resume a natural state of wellbeing.
Stress and Trauma in the Body
Paul Mclean’s Triune Brain Theory helps us to understand the difference between top down (CBT, psychoeducation) and bottom up (Somatic Experiencing, Trauma Informed Yoga) interventions by illustrating how three distinct levels of brain development inform the neurobiological process (Holden, 1979). Considered the first and oldest area of the brain is the reptilian, or R-Complex. The R-Complex dates back to the ancient reptiles and is responsible for self-preservation. The reptilian brain houses the brain stem and cerebellum and activates the Autonomic Nervous System (ANS) to manage the basic biological functions needed for survival. Next is the mammalian (or social) limbic system, which acts as the center responsible for the processing of emotions, moods, expectations and meaning (Holden, 1979). The third most recent area of brain development is the neocortex. The neocortex is where we do most of our thinking and it is responsible for higher levels of executive functioning. When threatened, the reptilian brain activates the nervous system, and the call to action causes the body to brace and produce extra energy to prepare for the danger (Holden, 1979).
This hyper-vigilant function instigated by fear centers of the brain will then begin to create memories that lodge into muscle tissue and become a source of continually activated tension until it is discharged. Recent events threatening our existence and disrupting our lives may activate a stress response that leads to deregulation of the ANS and a disorganized mind-body connection. For some people the fear response will cause the amygdala center of the brain to continually trigger the hypothalamus so the Sympathetic Nervous System (SNS) becomes over-activated and goes into fight or flight mode (Sherin & Nemeroff, 2011). In this state, the body will produce catecholamine neurotransmitters such as dopamine, epinephrine, and norepinephrine causing clients to experience symptoms of rapid heartbeat, anxiety, insomnia, anger, generalized muscle pain, high blood pressure and headaches (Miller, et al., 2011). However, for others, the sustained stress will produce dysfunction of the parasympathetic nervous system (PSNS) through the Dorsal Vagus Nerve and lead to a freeze response (Sullivan et al., 2018). The immobilization reaction will then decrease muscle tone and cardiac output and lead to symptoms of low blood pressure, extreme fatigue, memory loss, depression and disassociation.
Various degrees of fluctuation between the fight, flight, and/or freeze response will also cause dysfunction at the Hypothalamic-Pituitary-Adrenal (HPA) axis and create a faulty neuroendocrine feedback loop to over and under-produce thyroid, adrenal (cortisol), growth, corticotrophin-releasing (CRH) and adrenocorticotropic hormones (ACTH) (Sherin & Nemeroff, 2011). Dysregulation of the HPA axis can have a deleterious effect on our mental health as well as bring on medical conditions that may not resolve without a way to rebalance the system. Daniel Siegel defines the mind as the “embodied and relational, emergent self-organizing process that regulates the flow of energy and information” (Neukrug, 2015). Thus, when trauma has caused the mind and body to become unbalanced, wellbeing cannot be attained until integration is restored. Somatic therapies can help reduce dis-ease caused by tension and improper neural activity through a renegotiation of the triune brain by starting from the bottom up. These embodied interventions focus attention on internal body sensations (interoception) as a way to first release stuck energy and restore equilibrium so that executive cognitive function can come back online and produce the clear thinking needed to reduce rigid and/or chaotic responses to trauma or stress.
Embodied Therapeutic Interventions
Social workers who are trained to be aware of the multidimensional connection between the human body and mind can provide treatment through a patient-centered strength based perspective. An attuned social worker with an underlying practice of loving-kindness can assist a client by providing a safe container to use yoga for processing negative energy stored in the nervous system (Warriors at Ease, 2015). However, embodied therapies can re-trigger trauma so it is important to go slowly and make sure to be fully available for a debriefing after each session (Warriors at Ease, 2015). If a therapist is uncomfortable using yoga as an intervention on his or her own, clients can be referred to a provider with specialized training who may be available for online sessions while we are physically distancing.
The goal of embodied therapy interventions is to produce integration of the mind and body through healthy Vagus nerve tone and congruent functioning of the ANS (Van der Kolk, 2006). Adding somatic therapies such as trauma informed yoga to a treatment plan can provide clients with an understanding of how bodily sensations are a form of communication designed to bring awareness of threat or unhealthy patterns of behavior while elucidating insight into feelings that contribute to comfort (Trauma Recovery Summit, 2020). Trauma informed yoga aims to create a space where clients are free to explore uncomfortable mind-body sensations from a place of safety and curiosity. The therapist, or yoga teacher, will use breath work to keep the sympathetic and parasympathetic nervous system in balance so clients can transition in and out of poses with a sense of calm (Sullivan et al., 2018). This breath work helps to create stability and supports awareness of thoughts and sensations as ascending and descending waves that eventually go away. This provides clients with an empowering internal resource for emotional regulation and a sense of self-control that can be accessed during exposure to extreme external stress (Sullivan et al., 2018).
Current events have required us to live through a time of trying to simultaneously negotiate the tension between a need for separation to fight COVID-19 and the requirement of mass union to end the insidious suffering caused by social injustice. So, how do we navigate this paradox in a way that allows us to show up and provide a safe container for therapies focused on integration of the body and mind during quarantine? Most of us are already in the process of adjusting to work from home and/or using technology as a new way to connect with each other. Once a safe place for therapy has been established, a therapist can help clients orientate to both on and offline environments by having them look around the room and name objects they see. This can be particularly beneficial for keeping the parasympathetic nervous system regulated in people with PTSD who tend to become disoriented due to disassociation.
The therapist can then assist a client with grounding into the present moment by directing attention to senses felt in the body. Asking a client to focus on the sensation of feeling their feet on the floor may help bring awareness of what is happening in the body while also obtaining a feeling of being securely rooted in the ground beneath their feet. This can support clients with feeling safe and connected in the present moment and reduce thoughts and feelings that cause anxiety. Trauma informed yoga often applies this kind of grounding principle through the technique of having a client lay with their back on the floor and their legs pressed up against the wall. The pose is very relaxing and also serves the pragmatic function of calming the sympathetic nervous system in people with a strong fight or flight impulse by keeping blood from pooling around the feet in preparation to run or go into battle. In yoga we may also use the metaphor “root down to rise up” in conjunction with Tree Pose as an illustration of balance and integration. We imagine our feet are rooted deeply in the ground while the arms flexibly sway with the wind. This symbolizes how to stay grounded and flexible at the same time and contributes to internal and external resourcing that creates flexibility and avoids rigidity during chaotic times.
Resourcing is the ability to attune to positive sensations in the body that make us feel safe, and the more we have access to positive internal and external resources, the greater our chance at equanimity and resiliency. Once the external environment is no longer threatening and a client has become oriented and grounded in a safe space where they feel empowered with some positive internal resources, the clinician can begin to facilitate a very gradual titration of the traumatic experience by slowly helping the client become attuned to negative internal body sensations. It is important to interact with this kind of interoception very slowly so that a client can develop feelings of comfort with the ebb and flow of the nervous system. Somatic Experiencing describes the state of the nervous system to naturally pulsate between contraction and expansion, or rest and action, as Pendulation (Payne, Levine, & Crane-Godreau, 2015). Clients should be helped to be attuned to the pendulation process very gently so the traumatic energy stored in the nervous system can be gradually titrated and discharged, often in the form of shaking or crying (Payne, Levine, & Crane-Godreau, 2015). The release will bring the sympathetic and parasympathetic nervous system back into balance and nurture the neurobiological re-organization necessary for trauma completion, the assignment of meaning, and an experience of post-traumatic growth (Payne, Levine, & Crane-Godreau, 2015).
If we are to produce any meaning from the COVID-19 pandemic, it is a deeper understanding of the importance of interconnectivity. When we foster integration by treating individual trauma, we also invite healing of the collective trauma brought on by social division. Transitions are never easy; however, the more awareness we bring to the fact that we are biologically wired for interdependence and collaboration to ensure our survival, the more we advance collective healing. So, remember to breathe and stay grounded in the internal resources that will empower you with more response-ability to help guide the paradigm in shifting toward a harmonious, just and equitable society.
For references please contact the author at cscswgla@gmail.com
Emily Plain earned her MSW from the University of Southern California and has specialized training and certifications in Trauma Informed Yoga, Yoga and Mindfulness for PTSD, Yoga for Veterans and Yoga for Military Sexual Trauma. She currently holds positions at the West Los Angeles Department of Veteran’s Affairs and the Santa Monica Center for Acceptance and Change. She also serves as the Greater Los Angeles District Coordinator at the California Society for Clinical Social Work. She can be reached at: cscswgla@gmail.com
Burnout, Secondary Traumatization, and Healing in the Time of COVID-19
 By Nikola Alenkin, Ph.D., LCSW
By Nikola Alenkin, Ph.D., LCSW
Today’s realities of living in a pandemic with constant stress, feelings of anxiety, and enmeshed personal/professional roles offer social workers opportunities for constructive change both personally and in the workplace. These prolonged stressors can create changes in our physical and mental wellbeing. Now is the time to integrate self-care principles into our lives, and to address organizational changes that emotionally support workers who may be feeling overwhelmed by their clients’ traumas and tragedies.
Stress in Social Work
Stress is omnipresent in our day to day roles as social workers. For many of us, we have experienced countless hours at work, clients who “zap” our energy, and the often time madness of bureaucracy. The work of Maslach in the 1970s identified the phenomenon of “burnout” (Maslach, 1976). In the 1980s, professional literature sought to expand these concepts and developed constructs such as Secondary Survivor (Remer & Elliot, 1988), CoVictimization (Hartsough & Meyers, 1985), and Savior Syndrome (NiCathy, Merriam & Coffman, 1984). These constructs, however, did not fully capture the impact of work with traumatized populations.
Professional literature and research regarding work with traumatized populations reached a surge in the 1990s. The work of McCann and Pearlman expanded the knowledge base of this work. Vicarious traumatization was expanded to describe symptoms that are experienced by professionals who work in varied settings with diverse client populations. It has been defined as “…the [permanent] transformation in the inner experience of the therapist that comes about as a result of empathic engagement with clients’ trauma material” (Pearlman & Saakvinte 1995, p. 31).
Figley’s (1995) Secondary Traumatic Stress has emerged as a construct that can fully capture the impact of work with traumatized populations. Secondary traumatic symptoms develop as social workers hear many traumatic stories and may become overwhelmed by their genuine feelings of empathy and caring. Figley notes that some professionals prefer to use the term “compassion fatigue” rather than “vicarious traumatization” or “secondary traumatic stress,” as it is less derogatory. Despite these debates, Figley’s contribution to stress literature is important because his construct is the only one that incorporates the elements of energy depletion common in work with traumatized populations. It is unique and fully captures the impact on some mental health professionals as it takes into account both energy depletion, as well as other personal and professional impacts.
Focus on Healing on Self and the Work Environment
How do we develop practices of self-care that not only make an impact on our stressors but are also integrative to our personal and professional roles? We can begin with a thorough assessment of our current stressors. A good place to start is with introspection and completing the ProQOL 5 (Stamm, 2009) measure https://www.proqol.org/uploads/ProQOL_5_English.pdf. This measure is a 30 item, Likert-scale (1= “Never”, 5= “Often”) used to look at aspects of compassion satisfaction and compassion fatigue (aka Secondary Traumatic Stress). The author describes it as a “measure of the negative and positive effects of helping others who experience suffering and trauma” (Stamm, 2009). Information on the scales and scoring are located at https://proqol.org/uploads/ProQOLManual.pdf.
Another excellent tool is the Perceived Stress Scale (Cohen, 1994) https://www.mindgarden.com/documents/PerceivedStressScale.pdf. This 10 item Likert scale looks at how different situations affect our feelings and our perceived stress. Information on the scales and scoring are at https://www.ucdenver.edu/academics/colleges/medicalschool/departments/Anesthesiology/ Wellness/Documents/PerceivedStressScale.pdf.
Developing a personal plan that works for you may include some of the following:
- Create a space for your self-care practice. Within the office this can be a corner of a desk or a separate chair that you utilize only for self-care. Honor this space, make it yours, and use tools that will help stimulate wellness through visuals, sounds, smells, and even taste.
- Schedule your self-care. You may want to start with 5 minutes. Make an effort to schedule this time to focus on your self-care and nothing else.
- Do what works for YOU, honoring your intuition and wisdom. Yes, studies show that meditation, yoga, and other exercises are beneficial, but we are individuals and need to create a practice that works specifically for us.
- Maintain your practice. Through fire and ice, don’t give up! To help maintain your practice let others know (in fact, invite them to join in with you!). This “peer pressure” can help nudge you when you need it.
- Role with resistance and accept change. Change in our lives is the most constant thing.
Developing an Organizational Plan to Create an Emotionally Supportive Environment
Organizational resources that provide self-care are also vitally important in the management or prevention of stress. Using a “self-care” framework can allow organizations and administrators to focus on aspects of self-care practices and policies that promote well-being rather than contribute to stressful environments. These aspects are 1) workload and time management, 2) attention to professional role, 3) attention to reactions to work, 4) professional social support and self-advocacy, 5) professional development, 6) revitalization and generation of energy (Lee & Miller, 2013).
How do organizations integrate some of the principles above to increase self-care (in turn increasing compassion satisfaction) and help to mitigate stressors? The importance of time management and workload management are critical for staff. Organizations can assist in this area by reviewing caseloads and determining the severity of each client for the worker. This would ensure a “healthy” mix of high intensity and low intensity consumers. This is beneficial because a key factor in reducing stressors is the balance of the caseload or the proportion of time spent in clinical activities with a traumatized population. Chrestman (1995) notes that higher percentages of traumatized clients were associated with increased levels of dissociation, anxiety, and intrusive thoughts and images (is this what you meant by intrusion?) for the worker.
Attention to professional role is also a key area organizations can assist in mitigating stressors. Social workers’ professional roles are largely defined by their clients’ needs. This client centered orientation plays a large part in the stress response as experienced by professionals because of the empathic attachment inherent in the worker-client relationship. It is this inherent empathic “relationship” that poses stressors for the social worker. As the concerns for the stressors clients face become those that the social worker must resolve, the social worker’s stress may increase by virtue of the secondary experience of hearing or “working through” the issues with the client/consumer. (Bride, Radey & Figley, 2007). (Does this mean that the task of the social worker is to resolve the stressors, or that social workers think or feel they must resolve – I’m just not sure what this sentence means. If you’d like, you could give an example here.)
Using the supervision process to look at the mitigating stressors is important. Organizations can train supervisors in a compassion satisfaction model of supervision. This model, Enhancing Clinical Experience and Reducing Trauma (CE-CERT), (Miller & Sprang, 2016), utilizes a five component model: (experiential engagement, reducing rumination, conscious narrative, reducing emotional labor, parasympathetic recovery.) , It provides a good basis for the supervisor (and in turn the organizations) at a larger level) to “allow the clinician to remain emotionally regulated during treatment and, will, therefore, reduce compassion fatigue.” Organizations would be better served by training their supervisors and managers in this model to mitigate stressors within their staff.
Professional support and advocacy can be integrated throughout the work of the organization. Development of case conferences to allow front line workers and supervisors to share best practices are an easy way to start. Development of a self-care program within organizations where peers come together to practice self-care are also effective (Alenkin, 2020). On-going and consistent training for supervisors/staff are also effective ways to not only provide professional support but also professional development. Succession planning and mentorship programs are also cost-effective ways for professional development within organizations.
For example, whether the organization is small or large, providing consistent supervision in a safe and “open” environment (where the social worker feels comfortable to share and can be assured that they will be heard), helps with service delivery. In a former organization I worked in we added, “consumer victories” to every meeting. During this time, social workers were encouraged to share how they managed what was perceived as a difficult case and steps they took to get issues resolved or assistance to the person/family. Taking 15-20 minutes out of each meeting instilled comradery and also instilled hope that the work was meaningful despite perceived challenges. This went a long way to bring social workers (and other staff) together to hear about experiences and to be resourceful, it also focused on strengths rather than negatives.
(Would you like to give an example/short vignette or two about how some of these organizational changes have affected particular social workers – you can make it up. This is not necessary, but examples go a long way in helping people to understand and incorporate ideas – we are geared to learn from and remember the stories – more than abstract ideas.)
A Path Forward Towards Self-Care
The demand for social workers and social service delivery will increase in the coming years. As this demand rises, so too will the stress that these professionals will face. Individual social workers and organizations that utilize self-care methods for their staff can create environments where self-care becomes second nature to the work environment and the resulting impacts of reduced stress will help in facilitation of service delivery. Organizations can begin to implement programs with little cost and time expenditure. Our critical roles as change agents are not only meant to be utilized toward our clients and groups, but also within organizations and institutions as well. We can employ our skill sets as advocates to create better work environments for ourselves and our colleagues. The path forward towards self-care begins with us.
For References, please contact the author at nalenkin@yahoo.com
Dr. Nikola Alenkin, LCSW, has been in the field of social work for 25+ years. His clinical experience includes administration/management of programs within the public and private sector, along with direct practice to specialized populations. He is an educator of social work, psychology, and child/family studies for the past 20+ years. He conducts research and is a sought-after speaker in the areas of stress and coping, homeless population service delivery and work with specialized populations (transgendered, chronic mentally ill, prior incarcerated individuals). He is co-founder/ co-director of a community organizing and policy advocacy institute (California Organizing and Policy Institute) https://youtu.be/kdv9Z80z-oA and also has a resource YouTube page for social workers (Social Work Wisdom) https://youtu.be/c3W5-rSP6pk. He also provides consultation in training and organizational strategy throughout Los Angeles. Contact nalenkin@yahoo.com
.jpg) Is Casual Sex an Essential Service?
Is Casual Sex an Essential Service?
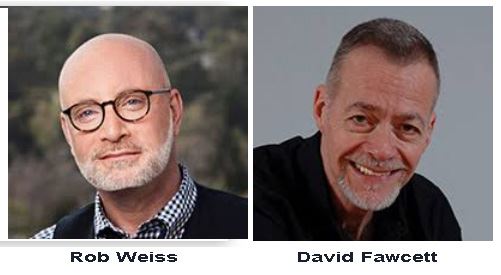
Robert Weiss PhD, LCSW
This article was originally published on PsychologyToday.com at this link (https://www.psychologytoday.com/us/blog/love-and-sex-in-the-digital-age/202004/is-casual-sex-essential-service). It is reprinted with permission of the author.
Tagline: In the midst of a pandemic, why do casual sex apps continue to operate?
In 1990, as a newly minted social worker, I was invited to present at a San Francisco-based HIV/AIDS conference about what we now refer to as Compulsive Sexual Behavior Disorder and its relationship to the transmission of HIV. At that time, we had few solutions for people with HIV/AIDS. They mostly got sick and died. So this was a matter of life and death for the gay community.
Back then, I was a young, passionate, highly engaged therapist who sincerely wanted to combat HIV/AIDS. That’s why I was giving this talk – a talk that eventually became my first book, Cruise Control (now in its 2nd edition). But this was my first talk in front of a professional audience, and I was completely terrified. How would they receive me? Would they hear and accept my message about the need for sexual behavior change to curb the HIV/AIDS pandemic?
Well, it didn’t go well. The moment I began to express concern about having just walked in on some men having sex in one of the bathrooms in the hotel where this very conference was being held, the boos began. And then the catcalls. “You’re just like those jerks who closed the bathhouses,” and, “Go back to your effing conservative life, you homophobic jerk.” Such was my reward for calling out sexual behavior (occurring right down the hall) that was contributing to the HIV/AIDS crisis. To my audience, individuals who were considerably more attuned to social bias and prejudice than medical science, my message was misperceived and unwelcome.
Well, here we are 30 years later, facing another deadly virus transmitted through close physical contact. And here I am again, voicing a professional message of concern about the possibly deadly impacts of casual sex. But this time I am prepared for, ready for, and even anticipating backlash. I fully expect that some readers will strongly disagree with what I’m saying in this blog, and they will wonder how I can be so sexually conservative, judgmental, unsupportive, anti-sex, and all the rest.
If you are one of these folks, let me respond with the same answers I gave in 1990.
- Our health and survival are more important than what you think of me or my words.
- Your right to have in-person casual sex does not trump the greater needs of public health.
- Calling out sexual behavior that promotes potentially lethal virus transmission is not sexually conservative; it’s simply the right thing to do.
In 2020, instead of talking about men having sex in bathroom stalls, I am asking why, when I can’t walk down the street without wearing a facemask, are hookup apps still helping people geolocate partners for casual sex. Sure, some of these services have posted warnings – brightly colored, occasionally flashing statements that essentially say, “Don’t do what you came here to do, it’s not a good idea.” But after that, you are free to hook up for casual sex with any interested person. So the real message is more like, “Have fun and try not to die.” Much like the warnings we put on cigarettes.
It is not now nor has it ever been my job to judge the sexual choices and behaviors of consenting adults. I am not the sex police, and I don’t want to be the sex police. In actuality, I’m pretty darn sex-positive. But today, as during the HIV/AIDS crisis, lives are on the line. In the midst of a lethal virus outbreak, some of our social and sexual freedoms must take a backseat to public health. When facing a disease for which we have no vaccine or cure, perhaps even the horniest among us should step away from casual sex for a while. And maybe the apps that help and even encourage people to hook up for casual sex should suspend that service until the pandemic passes.
I don’t know if such change requires legal action or a public health message or companies just deciding to do the right thing. What I do know is that there are plenty of sexual alternatives. For example, hookup apps could suggest and facilitate sexting and webcam encounters rather than in-person sex. Of course, nobody can stop others from engaging in face-to-face casual hookups. That’s as true now as it was during the HIV/AIDS crisis. But can’t we at least suggest some less-dangerous alternatives?
It may surprise you to learn that in ‘normal times’ I think these apps are a useful way for people to find one another. It’s also true that some of these services have evolved into more than hookup apps, becoming “adult friend finder” apps that help people connect for fun, friendship, and community. That said, these services are still primarily used to facilitate in-person casual sex, and they should do the right thing by either shutting down or pushing members toward alternative sexual behaviors. Helping people hook up for in-person sex is NOT an essential service. Not during a pandemic. And it needs to stop.
If you’re partnered, this is a great time for reconnecting with your spouse at home. If you’re single, it’s a great time for sexting, webcamming, and lots of other fun sexual behaviors. This is not, however, a great time for in-person casual sex.
For some, walking away from casual in-person sexual encounters, even for a short while, may be difficult, just as it was for certain people during the HIV/AIDS epidemic. For others, it’s no big deal. Either way, in the era of COVID-19, avoiding in-person hookups is not a discussion; it’s a public health imperative.
Once again, I don’t believe it is my or anyone else’s job to judge any adult’s consensual sexual choices. Now, however, like every other citizen of the world, I want to see this virus thing end. ASAP. I want this disease to go away. I want all of us to live long enough to have all the sex we want with whomever we want. But let’s have all that fun later, when we’re in the clear. Until then, let’s turn off the apps and stay away from in-person casual sex. If this sounds awful to you, I urge you not to worry. Try some of the fun alternatives suggested above as a stopgap, and know that all those hot in-person hookups will be there for you when COVID-19 has gone away.
Robert Weiss PhD, LCSW is Chief Clinical Officer of Seeking Integrity LLC, a unified group of online and real-world communities helping people to heal from intimacy disorders like compulsive sexual behavior and related drug abuse. He led the development of Seeking Integrity’s residential treatment programming and serves on the treatment team. He is the author of ten books on sexuality, technology, and intimate relationships, including Sex Addiction 101, Out of the Doghouse, and Prodependence. His Sex, Love, and Addiction Podcast is currently in the Top 10 of US Addiction-Health Podcasts. Dr. Rob hosts a no-cost weekly Sex and Intimacy Q&A on Seeking Integrity’s self-help website, SexandRelationshipHealing.com (@SexandHealing). The Sex and Relationship Healing website provides free information for addicts, partners of addicts, and therapists dealing with sex addiction, porn addiction, and substance abuse issues. Dr. Rob can be contacted via Seeking Integrity.com and SexandRelationshipHealing.com. All his writing is available on Amazon, while he can also be found on Twitter (@RobWeissMSW), on LinkedIn (Robert Weiss LCSW), and on Facebook (Rob Weiss MSW).
 The Plague? We’ve Been Here Before
The Plague? We’ve Been Here Before
by: Robert Weiss, PhD, with David Fawcett, PhD
This article was originally published on PsychCentral.com at this link (https://blogs.psychcentral.com/sex/2020/04/the-plague-weve-been-here-before/). It is reprinted here with permission of the author.
Death and dying? Yup.
Shock, anxiety, and confusion? Yup.
How could this happen? Yup.
Government late to the problem and lacking solutions? Yup.
Raw fear? Yup.
Hospitals overflowing? Yup.
Uncertainty about who is well and who is not? Yup.
Lack of clarity regarding transmission and lethality? Yup.
As gay men of a certain age, my colleague Dr. David Fawcett and I are having some uncomfortably familiar feelings. Déjà vu, if you will. You see, we’ve already lived through a plague – in this country, in our lifetimes. We’ve seen sickness, overflowing hospitals, and death on a mass scale. And to be honest, we were hoping those experiences would occur only once in our lifetimes. But apparently not. Because here we are again.
There was a time, not so long ago, when nearly everyone we knew was afraid of a potentially deadly disease that they didn’t understand, with symptoms that didn’t manifest immediately, sporadic testing, and no cure. It was a time when none of us knew who did and who didn’t have a lethal and easily communicable disease. People were dying – quickly, unpleasantly, far too young. We had no idea how to stop the spread, and our government failed to grasp the enormity of what was happening. So we watched helplessly as countless friends and loved ones grew sick and died.
For most of America, the early-1980s were pretty awesome. Wham, Madonna, Whitney, Prince, and Michael. The mall, bright colors, big hair, and all-night dance parties. Other than the constant fear of nuclear holocaust, life was relatively simple. Until the plague. Which not everyone experienced. Many people died or loved someone who died. But much of our nation never got closer to the epidemic than listening to Dan Rather on the evening news.
For the most part, AIDS was viewed as a “gay virus,” and the majority of the American populace was not at risk. Our current plague started in similar fashion, initially labeled the “Chinese virus” by government officials and others who were eager to distance themselves and to declare themselves and other God-fearing Americans as immune to all things bad or painful or deadly. “Not me. Not us. Nothing to worry about here.”
Then we found out COVID-19 is an equal-opportunity disease.
For people who lived through and remember the unimaginable horrors of the AIDS epidemic, the current pandemic is creating some post-traumatic stress symptoms. We remember crossing names out in our address books until there were hardly any names left. We remember going to memorials three times a week. We remember when we were so wounded, so damaged by all the death and dying that we decided we would no longer go to memorials. We simply had no tears left.
We also remember a sense of us and them. In the 1980s, the White House, the social elite, and much of America embraced expensive tastes, extravagant events, gigantic shoulder pads, and a culture of self-absorption. Our favorite TV show was Dynasty. “Greed is good” was more than a line from a movie; it was a mantra. And I have to ask: Are we much different today, with government geared toward the rich, massive drug-fueled ‘circuit’ parties, $1500 skinny jeans, and Keeping Up With the Kardashians?
In the 1980s, it was the “4H Club” that was dying: Homosexuals, Haitians, Heroin Addicts, and Hemophiliacs. Right wing politicians and religious leaders used this to foster discrimination and stigma, and as the rationale for ignoring the epidemic and letting the disease run its course with little or no intervention. They actually said hateful things like, “AIDS is a punishment from God,” and, “These people brought this on themselves, so why should we try to help?”
With coronavirus, of course, it’s a little different. It’s the “E Club” that’s sick and dying: Everybody. Our grandparents, parents, siblings, children, friends, and neighbors. It’s not just people on the margins. Rich people are getting this disease. Even rich and famous people are getting this disease. Powerful politicians, too, like UK Prime Minister Boris Johnson, who spent several days in an ICU as he battled the disease.
In the 1980s, the names of famous people suffering with and succumbing to the pandemic shocked the public into a growing awareness that a plague was truly afoot. Yet there was still a belief that the virus was a problem of “others” that would never hit home for most. This presents yet another parallel with COVID-19, with the federal government and numerous states loosening (or completely failing) to implement shelter in place orders and countless people in states with such orders choosing to ignore them or even protesting against them.
David and I have witnessed firsthand the effects of a plague. During the AIDS epidemic, we both lived in New York City, and we can still picture young men on the streets in the West Village – blind from cytomegalovirus, skin marred with Kaposi’s Sarcoma, frail beyond words, many experiencing dementia. These beautiful, dying men still haunt our dreams. Today, of course, the afflicted gasp their last breath hidden away in ICUs, under anesthesia and quarantined from loved ones. Only the wailing of ambulance sirens and the presence of refrigerated trucks at the delivery bays of hospitals belie the enormity of the still-growing death toll. But make no mistake, people are dying just as fast, if not faster, than we saw at the height of AIDS.
This virus is less discriminating and more easily transmittable than HIV, yet there is still denial among our leaders and much of the population. Parties at the beach, family gatherings, religious celebrations, and plenty of other events are still taking place – sometimes okayed by the state, sometimes not. And this reckless self-absorption is having deadly consequences, not only for those who are reckless but for their loved ones, their friends, and even total strangers.
Surprisingly to us, there are a lot of people who seem to think that nothing like this has ever happened before. But in reality, this is far from new ground. People are getting sick and we’re struggling to test them. People are dying and we don’t know how to stop that. Our hospitals are overflowing and medical personnel are putting their lives at risk to care for those who are ailing. And our leaders are blaming everyone but themselves for the lack of leadership in a time of extreme national crisis. It’s déjà vu all over again.
Maybe this time we’ll learn something that will help us be better prepared for the next time.
Robert Weiss PhD, LCSW is Chief Clinical Officer of Seeking Integrity LLC, a unified group of online and real-world communities helping people to heal from intimacy disorders like compulsive sexual behavior and related drug abuse. He led the development of Seeking Integrity’s residential treatment programming and serves on the treatment team. He is the author of ten books on sexuality, technology, and intimate relationships, including Sex Addiction 101, Out of the Doghouse, and Prodependence. His Sex, Love, and Addiction Podcast is currently in the Top 10 of US Addiction-Health Podcasts. Dr. Rob hosts a no-cost weekly Sex and Intimacy Q&A on Seeking Integrity’s self-help website, SexandRelationshipHealing.com (@SexandHealing). The Sex and Relationship Healing website provides free information for addicts, partners of addicts, and therapists dealing with sex addiction, porn addiction, and substance abuse issues. Dr. Rob can be contacted via Seeking Integrity.com and SexandRelationshipHealing.com. All his writing is available on Amazon, while he can also be found on Twitter (@RobWeissMSW), on LinkedIn (Robert Weiss LCSW), and on Facebook (Rob Weiss MSW).
REVIEWS
Book Review: White Fragility, by Robin DiAngelo
 Reviewed by: Dr. Chaz Austin
Reviewed by: Dr. Chaz Austin
Published by Beacon Press, 2018. 169 pages.
ATTENTION ALL WHITE LIBERALS: YOU ARE A RACIST.
What’s that? Not you? You’ve fought for racial equality your entire adult life. You’ve marched, protested, donated. You think I have you confused with some redneck from the Deep South.
Robin DiAngelo’s “White Fragility” is one of those books that, provided you are willing to part with your preconceptions, doesn’t simply supply more interesting information, but addresses that which you don’t know you don’t know. It was she who coined the term, “white fragility” in 2011, defined as white people becoming defensive/angry/hostile when accused of being complicit in systemic racism.
“The most effective adaptation of racism over time,” DiAngelo says, “is the idea that racism is conscious bias held by mean people.” This ‘good/bad binary,’ the world split into evil racists and compassionate people of tolerance, is in itself a racist construct. White “liberals” can’t face the fact that they share the responsibility for perpetuating this. Yes, every one of them. “I believe that white progressives cause the most daily damage to people of color,” she says.
DiAngelo, who is white, and has run diversity-training workshops for over 20 years, shows us that white people have always been privileged. So much and for so long, that we don’t even realize how lucky we are. She says that we need to become conscious of our own sense of entitlement before we can effectively change the status quo of institutional racism in this country. “If we cannot discuss these dynamics or see ourselves within them, we cannot stop participating in racism. The good/bad binary made it effectively impossible for the average white person to understand— much less interrupt— racism.”
“Color blindness,” the belief that race doesn’t matter (in other words, white people who say they don’t see race), is exactly what stands in the way of our dealing with the fact that it actually does.
According to DiAngelo, the constructs of race under which Americans live began when Europeans started colonizing the New World. White colonizers stole indigenous peoples’ lands, and needed to create a reason to justify treating these people of color as less than human. This is when racism and illusion of white supremacy began. Race – and racism are social, not biological in origin.
It’s about power over other people. As President Lyndon B. Johnson once said, "If you can convince the lowest white man he's better than the best colored man, he won't notice you're picking his pocket. Hell, give him somebody to look down on, and he'll empty his pockets for you."
White people unconsciously view whiteness as normative, and only value white culture and traditions. For example: ’‘flesh colored’’ makeup, the flesh always being white flesh; Jesus, who lived in the Middle East and most certainly was not white, is almost always depicted as a white man; “primitive” art, etc. I have a cousin who is a concert pianist and rejects music created anywhere but in Europe or the United States as simply “not music.” In this model, whiteness is the benchmark against which all other races are measured. Most white people cannot confront the fact that they have bought into this.
As the diversity educator Jane Elliott said to a roomful of participants in one of her workshops: “If you as a white person would be happy to receive the same treatment that our black citizens do in this society - please stand! . . . You didn't understand the directions. If you white folks want to be treated the way blacks are in this society - stand! . . . Nobody is standing here. That says very plainly that you know what's happening. You know you don't want it for you. I want to know why you are so willing to accept it or to allow it to happen for others.”
But there is hope. As DiAngelo says, “I have found it much more useful to think of myself as on a continuum. Racism is so deeply woven into the fabric of our society that I do not see myself escaping from that continuum in my lifetime. But I can continually seek to move further along it . . . This idea changes the question from whether I am or am not racist to . . . am I actively seeking to interrupt racism in this context?”
This is the challenge white people face – to wake up. And stay woke.
Dr. Chaz Austin, Ed.D. is a New York Liberal Jew who has lived in Los Angeles for the past 40 years. His latest book is “101 Ways to Find Work . . . and Keep Finding Work for the Rest of Your Career." He can be reached at chaz@chazaustin.com.
Book Review: Trans Kids: Being Gendered in the Twenty-first Century by Tey Meadow
 Reviewed by: Holly Wood, Ph.D.
Reviewed by: Holly Wood, Ph.D.
Published University of California Press in 2018. 300pp.
Summary/key Points
In her work, Trans Kids: Being Gendered in the Twenty-First Century, author Tey Meadow performs ethnographical research by interviewing transgender adolescents, their parents, and activists to explore the contemporary gender moment and what it means to be “gendered” in the Twenty-First Century. Meadow notes that ‘gender identity,’ or the felt sense of gender, is fundamental, immutable, and not tied to the materiality of the body, but rather, is part of an intricate social practice that is influenced by individuals, families, and larger social systems. Therefore, we are encouraged to understand that gender nonconformity constitutes social identity, rather than an erosion of the gender system. She effectively uses her gathered research as well examining her own role in the study to argue that gender isn’t merely performed, but it is also given. She also argues that contrary to popular feminist theorist attempts to eliminate gender categories in efforts to liberalize gender restrictions, the proliferation of the current gender movement and acceptance of mobility between categories does not necessarily destabilize the categories themselves, but instead, allows for the institutionalization (and, contemporaneously, the acceptance) of categories beyond the binary. In other words, transgender children of the 21st century offer us an opportunity to examine gender beyond the categories of male and female, and instead challenge us to acknowledge the social processes that influence a person’s gender identity.
A short appraisal of the strengths and weaknesses
Meadows’ work left me in admiration of its strengths and scraping for crumbs of weakness. It is well-written, easy to read, and entertaining. The book is clearly organized, which lends to its ease of reading. The author does an excellent job of blending theory and practice, and utilizing academic theory in a way that is easy to digest by wider audiences. The work is thoughtful and well-researched, especially in how the author uses reflexivity by clearly understanding and explaining how her own existence impacts the social processes of gender and thus, the research itself. As far as weaknesses, I wish there were more voices from the adolescents themselves, though I understand and admire Meadow’s reason for not doing so as she notes not wanting to unintentionally damage or pathologize adolescent participants.
However, the lack of children’s voices is made up by the personal accounts from parents, which further highlight adults’ roles in navigating the social spaces of their trans-identified and gender-nonconforming children. Parents detail how they navigate social structures, school systems, participate in activism, and construct different sets of rules for their child's public life than they maintained within the walls of their homes. Families revised institutionalized tropes and reimported them back into the institutions they inhabited; in that way, they made social change. They offer a glimpse of integration: how people reformulate their understandings of the world in response to queer lives. They bring clarity to the processes by which individuals make dissident identities and articulate how they challenge and reinterpret dominant frameworks to support their children.
This book is an excellent resource for clinicians who want to better understand their gender non-comforming clients and how they navigate the world. This work would also serve as being exceptionally powerful for parents of trans- and gender-nonconforming children as much of the book includes first-hand narratives of the trials, tribulations, and love of parenting a transgender child. Furthermore, this book adds to scholarly work on gender by providing a fresh take on something: the first generation of gender nonconforming children. Meadow achieves her goal of examining the social processes in which gender is embedded, performed, and given, and does so in a way that is supportive and non-pathologizing.
Overall, I think it opens our eyes to changing meanings of gender, the social processes that influence a person’s gender identity, and what it truly means to be gendered in the 21st century. Thus, leaving the reader with hope for the institutionalization and acceptance of categories beyond the binary.
Tey Meadow is an associate professor of sociology at Columbia University, where she teaches courses on gender and sexuality, queer theory, qualitative methodology, law, and the analytics of risk and uncertainty. Meadow’s published work focuses on a broad range of issues, including the emergence of the transgender child as a social category, the international politics of family diversity, the creation and maintenance of legal gender classifications, and newer work on the ways individuals negotiate risk in intimate relationships.
Holly Wood is a Los Angeles based Sex Therapist, EMDR trained Trauma Specialist, and Clinical Sexologist specializing in trauma, sex, and intimacy concerns. She is currently pursuing her PhD in Human Sexuality from the California Institute of Integral Studies, focusing on sexual trauma and social justice. Holly is committed to sexual wellness by working with clients to get past their past and develop the necessary skills to achieve lifelong change for a more pleasurable and connected life. She can be reached at (951)394-1285 hollywoodmft@gmail.com and https://www.hollywoodmft.com/
Documentary Review: 13th (on Netflix)
 Reviewed by: Jean Rosenfeld, LCSW
Reviewed by: Jean Rosenfeld, LCSW
13th “In this thought-provoking documentary, scholars, activists and politicians analyze the criminalization of African Americans and the U.S. prison boom. This piercing, Oscar-nominated film from Ava DuVernay won Best Documentary at the Emmys, BAFTAs and NAACP Image Awards.” (Netflix description)
For an historical and political understanding of the current Black Lives Matter protests, watch this documentary. It is as riveting as it is informative. Following are some of the highlights…
13th lays out how it has come to be that 25% of the world’s prisoners are in the United States, and that African Americans, who are 6.5% of the population, comprise 40.2% of prisoners. It begins with explaining that there is a loop hole in the 13th amendment ending slavery that allows involuntary servitude of prisoners. The rebuilding of the Southern economy after the civil war was in large part accomplished by incarcerating former slaves for minor infractions in order to use them as free labor. The 1915 blockbuster movie, Birth of a Nation, (that depicted black men as rapists) was influential in reinvigorating the Ku Klux Klan and fueling lynching and segregation. The documentary explores the backlash to the civil rights movement led by Nixon, the “Law and Order President,” who used “crime” as a stand-in for race, greatly increasing federal funding for police and prisons. He named drug abuse as public enemy #1, branding African Americans as heroin addicts, as well as hippies and anti-war demonstrators as pot heads. Reagan’s War on Drugs led to cutting budgets for health, safety net and social welfare programs and increasing funding for law enforcement and prisons, while giving tax breaks to the wealthy. The Clinton era saw 100,000 more police on the streets and the establishment of the Three Strikes Law and minimum sentencing; this built the infrastructure for the incarceration that we now have.
We learn about the American Legislative Exchange Council (ALEC), an organization of global corporations and state politicians who write “model bills” that directly benefit huge corporations. Among other industries they represent the prison industrial complex and write legislation to support private prisons by increasing the number of prisoners and the length of their sentences. One example is the Arizona law SB 1070 that led to the imprisonment of immigrants and undocumented citizens to fill the “detainment centers” (private prisons). This industry is not only comprised of the prisons and staff, but also telecommunication services that charge exorbitant rates for phone calls, food service, health care, uniforms, etc. Prison labor has served many industries as varied as Victoria’s Secret and Idaho potatoes. The Corrections Corporation of America, the largest provider of private prisons, is preparing for a downsizing of incarceration by gearing up to provide GPS monitors for home detention along with parole staff. Ninety-seven percent of indicted persons accept plea bargains because they cannot afford bail and are threatened with very long sentences. They not only go to prison but face a future after prison that greatly curtails their right to vote, employment, loans, housing, insurance and public assistance. The film ends asking the question of how is it we are accepting mass incarceration when we declare we never would have accepted slavery or segregation.
Jean Rosenfeld, LCSW treats adults in her private practice in Carmichael. She co-leads a consult/support group for beginning therapists and is editor of this newsletter. She is author of Therapy Cracks Me Up! Cartoons about Psychotherapy available on Amazon - CLICK HERE
Real Talk
by: Jaya Roy, M.A., ASW
This article was originally published on Jaya Roy’s blog at https://www.kantimentalhealth.com/post/
how-mindfulness-can-help-in-healing-from-racism - It is reprinted here with the permission of the author.
How Mindfulness Can Help in Healing From Racism
There is an eagerness and sense of urgency to address and eradicate racism in our newly awakened community members that is unsettling and alarming to the Black, Indigenous, Mixed Race, People of Color (BIPOC) communities that have been entrenched in this work for centuries, decades, and years. What we know is that racism is the air we breathe, the water we drink, and the very fabric of our society. To do this work means taking a whole new approach and having long term, sustainable action to dismantle oppressive systems while centering the work from our BIPOC community. What is often also unnerving is the inability or unwillingness for folks to internalize that we all act in ways to uphold racism, it's not just the people we see in the videos (hello Karen). The way we approach social justice work is just as important as the work itself.
I find myself having trouble discerning what spaces help me thrive, what spaces are uncomfortable, and what spaces are simply toxic. As a POC with experience and expertise in clinical social work and social activism, I have been inundated with organizations and individuals requesting anti-racism programing. In order to do this work and continue to do this work for my lifetime, it’s really important that I protect myself from further harm. We all know that good intentions and niceties do not supplant microaggressions.
While I know that true healing will come when we dismantle the systems (culture, policies, practices, etc…) that uphold racism, I find mindfulness to be a helpful tool to get me through the moment. I hope to share with my BIPOC community the ways in which mindfulness has helped me recently and a loving-kindness meditation I created specifically for BIPOC folks.
Mindfulness Can Be A Decolonized Practice
What is nice about mindfulness is that it has roots in Eastern Philosophies and cultures that sometimes resonate more with BIPOC communities. For example, many of the cultures that practice mindfulness hold a collectivist mindset whereas modern mindfulness in western countries often holds a more individualistic mindset. As a result, modern mindfulness sometimes disengages from the idea of community healing. Modern mindfulness is often presented as a way for the individual to manage emotions (how many times have you heard to do mindfulness when you feel stressed, anxious etc…). and frequently ignores how we can build our sense of awareness to not only better serve ourselves but also our community.
Mindfulness Helps Build Our Internal Racism Detector
We can practice bringing awareness to our thoughts, sensations, and emotions using mindfulness. This information is going to be key in helping us identify what spaces might we feel safe in, where we might feel challenged, and what is simply more toxic (something I’m practicing). Many BIPOC individuals internalize mental health in our bodies. Sometimes it’s a matter of being connected to your body and knowing what it’s signaling. For example, after meditating on experiences I’ve had, I’m starting to connect the feeling of my body suddenly dropping in space as a sign of possible emotional danger for me (cue in the Sunken Place clip from “Get Out”). Compared to when I feel challenged, my body feels more like I’m itching to get out of my skin - it’s uncomfortable but not alarming. This distinction helps me validate my own feelings and gives me clarity on how I want to exercise my autonomy in choosing spaces to do this work.
Mindfulness Is A Moment to Practice Loving Ourselves (in a world that actively does not)
There’s a lot of implicit and explicit signaling about Black and Brown minds, Black and Brown bodies. Our Black community, in particular, have experienced strong negative signaling with all the stereotypes of Black folks. Even the best of us internalize these messages whether it’s about our bodies, looks, or minds. Spending a few minutes to counteract the negative messages not only feels good but also aids in our critical understanding of things like body image, beauty, and intelligence, and white supremacy culture. Mindfulness is an opportunity to practice some loving kindness that we may not get elsewhere.
Mindfulness Is A Moment to Have A Break From The Bullshit
Lastly, it can simply be a way to be with your present self and in that moment and have a break from the microaggressions and so forth. Sometimes a break is the difference between getting through the day and falling apart (which it’s absolutely ok to do too).
Please check out my Loving Kindness Meditation that I use for my own practice: https://www.kantimentalhealth.com/post/how-mindfulness-can-help-in-healing-from-racism
Jaya Roy, M.A., A.S.W. is a Cognitive Psychologist and a Clinical Social Worker. She currently works at Mira Costa Community College as a Mental Health Counselor and serves as Chair for California’s Society For Clinical Social Worker’s (CSCSW) Diversity, Equity, and Transformation Committee. She is passionate about social justice and mental health, as well as the impact of the mind-body relationship on well-being. Jaya integrates frameworks from anti-oppressive practices, critical social work, and psychobiology in her clinical practice. When she is not focused on social work or activism, Jaya enjoys spending time with her birds, husband, or in the garden. kantimentalhealth@gmail.com https://www.kantimentalhealth.com/
 Jaya Roy, MA, MSW | Board Member and Diversity, Equity, and Transformation Committee Chair, CSCSW
Jaya Roy, MA, MSW | Board Member and Diversity, Equity, and Transformation Committee Chair, CSCSW
Associate Mental Health Counselor, Mira Costa Community College
Clinical Update: Thank you for being willing to share your experience with our readers. How did you decide to pursue a career in social work?
Jaya: I had pursued undergraduate and graduate degrees in Cognitive Psychology and did a lot of research. While I greatly enjoyed it, I also found myself feeling connected when I volunteered as a Crisis Counselor and mentored research assistants. I thought about shifting to doing more practice-oriented work. A colleague introduced me to social work. I appreciated that social work was more intentional in talking about issues of power, oppression, and privilege and considering group and societal levels.
CU: Could you tell me more about your work experience in the social work field?
J: I focus on integrating mental health and social justice. I have specialized training in Domestic Violence and Intimate Partner Violence and experience working in community mental health settings. I also worked closely with first generation students of color who face a lot of systemic barriers to education. At Mira Costa, I provide psychotherapy for students, I help facilitate support groups (LGBTQIA+), I’ve provided a presentation on emotion regulation, and in the future will be presenting at a conference with my supervisor on the topic of diversity and equity in the community college setting.
CU: Could you share more about common issues experienced by students you’ve worked with?
J: I work with very diverse students from different ages, races, socioeconomic statuses, etc. at Mira Costa College. I have found it to be similar to community mental health in some ways. There is such a range in terms of access to services. For some people this might be the only avenue to accessing mental health services. Most of the clients I work with experience some level of trauma such as homelessness, intimate partner violence, etc. We also see a number of students who are undocumented or first generation.
CU: Thank you for sharing your insights. What drew you to the field of college mental health?
J: So much of my professional life has been in academia or university and college settings. I really enjoyed working with individuals in this space. To me, students today experience so many challenges, including the astronomically high costs of education, so it is hard for many people, especially people with marginalized identities, to access education. It has never been easy, but I think it is even harder now. A lot of times these students are working two to three jobs to take care of their families. There is a cultural component as well where some students are responsible to not only do well at school but also take care of their families. In a college setting, especially at community colleges, there is a lot of focus on working with issues of equity and social justice, so it aligned with my practice orientation. If a therapist does not think about these topics, this environment might not suit them. A lot of people assume that students are coming to receive mental health services as a result of stress about schoolwork. It is often a small part of it. Students are facing such big challenges today. They are highly aware of the existential threat of the climate crisis, systemic racism, and now the pandemic, all while trying to get through class.
CU: How did you begin to engage in diversity, equity, and transformation work? Could you please share more about your experience and any advice for people interested in engaging in this type of work?
J: It is truly a lifelong journey to engage in social justice work. I have a unique lived experience because of my intersectional identities as a queer woman of color with physical disabilities and privilege of social economic status. Growing up it was hard to find words to describe my experience. When we don’t have ways to describe our experiences, we could potentially blame ourselves. I started to identify and create more awareness for my experiences, such as my encounters with racism and sexism.
When I was doing psychology research in the affective sciences I noticed there was little consideration of the role of systemic oppression and other experiences of social identities. I didn’t feel like we were getting at the heart of these topics. I also did not see a representation of diverse voices in academia, and academics hold immense power. I also saw that in our own research labs students would volunteer to get experience, it’s almost an unwritten requirement for gradschool, but several of them were starving, traveling from long distance in public transit and had no access to resources.
Even in the field of social work, there is a divide among social workers who see social justice topics as integral to our work and many that don’t. Despite social justice being in our ethics, there is not educational accountability reflecting this commitment and practitioners embodying these values to minimize harm. That is why I joined the Society. I’m looking for a place to push this initiative.
CU: Thank you very much for sharing your experience. What have been your favorite memories in your involvements with the Society?
J: I think getting to know other members with lived experiences as people of color has been a highlight. The Board has had some important, challenging conversations when we worked on strategic planning. The DET Committee has been working hard in building a sense of community despite our members living across the state of California. The personal relationships that I’ve built have been highly valuable to me.
CU: What words of advice do you have for social work students, early-career social workers, and social workers interested in learning more about the college mental health field?
J: I would tell social work students to be loud and not silent. Hold your values close to your heart. One of the things that I’ve learned over and over again is that the personal is political, even when we’re doing clinical work. Clinical work and political actions should not be separated, yet there has often been a falsely perceived dichotomy. Our field is not value-neutral. If we’re thinking about dignity for our clients, it has to go beyond psychotherapy. A part of psychotherapy might involve how we could help clients empower themselves and draw from their lived experiences to make social changes. That is the same for us as social workers. There are many important issues, such as the climate crisis, systemic racism, women’s rights, and health care that are at the forefront right now. As a field, we need to be prepared to talk about these issues and lead action on dismantling oppression in our society.
In the community college setting, it can be hard to get one’s foot in the door, but this is a very important area with high needs and a great way for an early-career social worker to gain training and diverse practice experience. I’d recommend those interested in the field to network and talk with people who are working in the field to learn more about what their work entails. Make sure you have realistic expectations. There can be a lot of trauma experienced by the client populations, so you must be willing to work with people who have had some tough experiences.
CU: Is there anything else that you’d like to share with our members?
J: Black Lives Matter needs to be movement. As Social Workers we have a prerogative to support and push this movement to the forefront as we have clear professional ethics of challenging all social injustice. We need to start with examining ourselves and our profession and the ways in which we have fostered anti-blackness. Social Work as a field has historically used access to resources as a way to support a few “deserving individuals” while the majority of communities are underserved. As individuals we may have the intention to support our communities but we need to critically evaluate our practices, policies, and culture and how together they all support to maintain the status quo. The status quo is not working. Book clubs and Facebook posts are one step in this work, but taking lifelong action is needed. For those of us that are not Black, it’s our job to use our privilege to bolster and uplift Black voices. We can start with examining our field. We need to ask ourselves what opportunities are we afforded because of our privilege. It might mean stepping aside and creating space for the Black and Brown voices to be heard. It might mean passing on jobs, speaking opportunities or more so more Black and Brown minds are in positions with power. Ultimately this is healing, and mental health goes beyond the one hour in the room with the client. I’m asking clinical social workers (and all social workers) to step up.
Wit and Wisdom
It's all so absurd - No human being is black or white. I have forty pastel colors that make up our skin, browns, yellows and reds, sand tones, flesh in every shade and nuance, blues and greens blended into shadows, And yet here we are, crushing, enslaving, using and abusing people for the pigments in their skin, the curl of their hair, their heritage or beliefs. For what? Is it Fear? Is it Greed? Power? A cruel Game? Whatever its cause, Its true name is Shame. |
Pastel portrait by Shauna L. Smith |
Shauna L. Smith, MSW, LMFT has been a family therapist in Sacramento for over 30 years. She is the author of the recently published memoir, Missing Father: A Daughter’s Search for Love, Self-Acceptance, and a Parent Lost in the World of Mental Illness. (to order: http://www.missingfather.squarespace.com) The pastel portrait, Momma and Baby, is from Child of My Dreams, an in-progress lullaby and book. Shauna can be reached atgushauna@yahoo.com
Jars – A Personal Reflection
 By Annie Wilson, LCSW
By Annie Wilson, LCSW
Is this a safe place for me to unpack my jars? I’ve been carrying them around for a while. Across time zones and state lines. I’ve tried to transform them through different environments and lifestyles. They grow heavy on my back and leave my thoughts distraught. I try to bend and disfigure them, but they are unchanging. They sit high on a wooden shelf in my mind. Pristine and unshaken. Glaring down, mocking my failed attempts to keep them hidden.
Once I dump out the contents of a jar, I don’t know what will happen to me. I fear I will lose myself to the powerful emotion the jar contains. The aching emptiness. The unrecognizable rage. The feeling of being numbingly apathetic. I’ve taken such delicate time packing these jars, so it’s easier for me to keep them closed. These intimate portions that make me who I am. Too complex for anyone’s eyes, including my own.
The trouble is, we can never really embrace this life without opening our jars. Handing its contents to another. Accepting their jars in return. Finding empathy in the mutual understanding of each other’s darkest experiences. Vulnerability breeds connection. But more important, and perhaps more fear-provoking, we must examine our own jars deeply and find unconditional love for ourselves, despite what they contain.
When we stop pretending to have everything put into place and embrace the wild, messy side of ourselves that we don’t yet trust, we begin to live. The more we run from ourselves the further away we get from where we actually want to be. Our jars will remain with us. When we try to ignore them, we slip into the same habits that lead to the same situations and we run into ourselves.
Often, the most terrifying and unnerving step into the unknown leads to the most gratifying reward. Sometimes you have to get lost within yourself, to find out who you are and what beautiful things you are capable of. It’s time to open the jars.
Annie Wilson, LCSW graduated from University of Georgia with her Bachelor’s degree in Social Work and from San Diego State University with her Master’s degree in Social Work. In addition to her work in the emergency department, she provides telehealth counseling to individuals with anxiety and trauma-related disorders.
What Will “Normal” Psychotherapy Become?: A Somewhat Cloudy Crystal Ball
 By Laura Groshong, LICSW, CSWA Director of Policy and Practice
By Laura Groshong, LICSW, CSWA Director of Policy and Practice
Just as we are settling in with videoconferencing and audio psychotherapy, the possibility that we will no longer be forced to maintain the distancing that led to these forms of practice is beginning to emerge. Here is my view of what we can expect in the near to later future, though it may vary from state to state and region to region.
Overview
Since the Department of Health and Human Services (DHHS) recently extended the state of emergency through October 25, it is likely that the current coverage of videoconferencing and audio therapy will continue as well. Medicare is likely to use the state of emergency as a guide for this.
Right now, however, there is widespread discrepancy in terms of which private insurers and self-insured or ERISA plans (Employee Retirement Income Security Act) will cover videoconferencing and audio psychotherapy, which insurers and ERISA plans will cover or waive co-pays, and which insurers and ERISA plans will pay for videoconferencing/audio therapy at the same rate as in-person therapy. While LCSWs used to feel frustrated by reimbursement rates, lack of coverage for more than once a week treatment, and treatment reviews for psychotherapy that lasted more than a year, we now have a whole new set of frustrations. Of course the anxiety we face about becoming infected or infecting others colors everything we do, rendering our insurance concerns less meaningful. But in a Beckettian way – “I can’t go on, I’ll go on” – we persevere and try to maintain our professional and personal lives. So here is what will determine whether the practice changes we have endured the past 6-8 weeks will become permanent, stay as ongoing new options, or be eliminated when the dangers of physical contact with others have waned.
One of the problems with predicting these issues is that states/jurisdictions are following such different trajectories in terms of the way COVID-19 is impacting the people who live there. “Hot spots” may be part of a state’s difficulty with the virus, while other areas are unscathed. Our state and local governments are trying to create guidelines that will protect as many people as possible, mainly through physical distancing, hand washing, wiping down all high touch surface, and masks. That is the legal “frame”; we all still have to determine what we think is safe in doing our work in the present and moving forward. I have heard from LCSWs all over the country and the vast majority have been conducting psychotherapy through videoconferencing and telephonic means for the past 3-4 months. Now: to address the confusion around insurance coverage of these new delivery systems.
What do we do when an insurer states they will cover the co-pays, pay the same amount for distance therapy as in-person therapy, describe which Point of Service (POS) code and modifier to use, and then fails to reimburse according to these stated policies? These problems are some of the most frustrating that we face. Spending hours tracking down provider liaisons about why our claim was denied, or paid at a lower rate, is painful and even scary. One remedy is to engage our patients in the process of finding out what their current co-pay coverage is. Keep a list of POS and modifier guidance as it comes out, by insurer, and keep it updated. If you find inconsistencies, let your insurance commissioner and attorney general know. This is the best way to get action on insurers’ failure to pay us what they have agreed to when we have complied with stated policies.
The Future of Telemental Health
As to the future: the most important decision will be whether Medicare agrees to maintain the expanded videoconferencing and audio psychotherapy until October 25 and/or after the current restrictions in physical distancing are removed. Their policy will impact most private insurers, according to my cloudy crystal ball. Since the current restrictions will be cut back on a state basis, it is hard to say when the Centers for Medicare & Medicaid Services (CMS) will decide there is enough safety to insist that Medicare beneficiaries be treated in-person. What I don't know is whether there will be an assessment of the videoconferencing and audio psychotherapy to determine whether they are as helpful as in-person treatment and how much more expensive it is to allow these forms of treatment to continue. CSWA will continue to work with CMS, HHS, and other Federal agencies to preserve the options that we now have, even after the crisis has abated. As you know, the predictions of when that will occur range from 6 months to 2 years.
In other words, use your own judgment about what practice system feels safe for you and your patients and let insurers know that they need to be consistent. Let your insurance commissioner(s) know if private insurers are unwilling to cover agreed upon and needed forms of treatment. And most of all - stay tuned.
Ms. Groshong is a Licensed Independent Clinical Social Worker in Seattle and has been in clinical private practice for the past 43 years. She was a Registered Lobbyist in Washington State for 25 years. She is the Director of Policy and Practice for the Clinical Social Work Association. She has written and lectured extensively on clinical and legislative issues around the country. She can be reached at lwgroshong@clinicalsocialworkassociation.org
IN MEMORIAM
CHARLOTTE SIEGEL, IN MEMORIAM
 By Leah Reider, LCSW
By Leah Reider, LCSW
Longtime CSCSW member, Charlotte Siegel, died in January at the age of 100. Charlotte was an active member of the steering committee for the Mid-peninsula district of CSCSW and in 2017 received a special award from CSCSW for “exceptional work that enhances the image of clinical social work.” The plaque which was presented to Charlotte stated: “With thanks for being a role model for generations of social workers and for your service to CSCSW and to the profession. Presented with gratitude and affection.”
Charlotte’s illustrious career spanned more than 60 years! She always brought both enthusiasm and a keen understanding of people to whatever job she undertook. She threw 100% of herself into her work and her relationships with people, and she thrived from both.
Charlotte began studies for her MSW at the University of Chicago and finished at UC Berkeley after moving to Stanford University with her husband, who was a renowned professor of anthropology. During the years between Chicago and Stanford, Charlotte had a number of medical social work jobs, but it was during a six-month stint at a VA hospital that Charlotte realized that psychiatric work was what interested her. Her husband encouraged her to return to school after having two children, though this was unusual at the time.
After completing her MSW, Charlotte went to work at Family Service Association in Palo Alto, where she worked for eight years. She then worked briefly at Stanford Medical School and went on to work for twenty years at Counseling and Psychological Services at Stanford. Because Charlotte had had many cross-cultural work experiences while her husband did his anthropological field work, she became a liaison staff person to Bechtel International Center at Stanford, where she helped numerous foreign students with their adjustment to life at Stanford.
After her twenty years at Stanford, Charlotte opened a private practice in Palo Alto. This was a big transition for Charlotte, who was used to working for social agencies. She grew to love her long-term work with clients.
When Charlotte moved into a senior residence, she set up and led a transitions group for about five years, from age 85-90. When she had an injury and was confined to the skilled nursing facility, she led the group from her bed. She saw her last individual client at the age of 95! The continuing theme in Charlotte’s life was about networking and connecting people with other people and with causes. In her eighties, she wrote a paper about her life as a social worker. Charlotte concluded her paper with the following statement: “My social work self, my clinical self, my total being self, they are all wrapped up together. There isn’t a separate clinician and separate Charlotte Siegel. It’s all a part of the definition and a part of what I am able to give to clients who come see me – a sense of life moving for me and for them.” We miss you, Charlotte.
About the Clinical Update
Editor: Jean Rosenfeld, LCSW
The Clinical Update publishes relevant, educational, and compelling content from clinicians on topics important to our members. Contributions and ideas for articles can be sent to jeanrosenfeld@gmail.com -- please write "Newsletter" in the subject line.
Ad placement? Contact Donna Dietz, CSCSW Administrator - info@clinicalsocialworksociety.org
.png)


